Stress Urinary Incontinence
Stress Incontinence is a common problem that affects the quality of life in affected people. In spite of being a widespread condition, it is under reported and also lot of women live with it for years before seeking help.
From the results of the largest epidemiological incontinence study to date (the EPINCONT study), the incidence of SUI is highest among women between 25 and 49 years of age. MUI (Mixed Urinary Incontinence) is more common in older women due to an increase in urge symptoms as well.
Fortunately, they can be managed by lifestyle modifications, pelvic floor exercises and if required surgery.
What is Stress incontinence ?
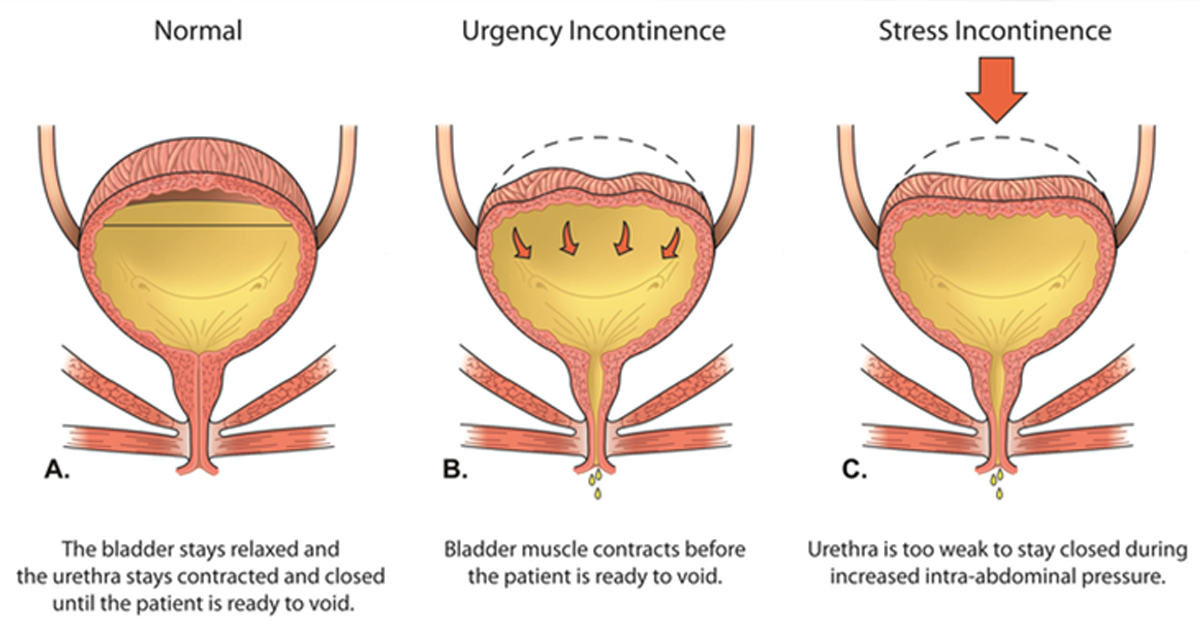
Leakage of urine during the times of increased abdominal pressure like coughing, sneezing, lifting, straining etc. Bladder normally holds urine until there is a desire to empty. In people with stress incontinence there is weakness of structure surrounding urethra and so urine leaks during straining.
How common is stress incontinence?
Overall, stress urinary incontinence (SUI) is the most prevalent type of UI, followed by mixed (MUI) and urge (UUI) types. It is the most common type of incontinence that women experience and can affect up to 40% of women. It is more common in older women with an average of 1 woman in 5 aged over 40 years old having some degree of stress incontinence.
What is the cause of Stress Incontinence?
There are several causes that increases the chance of developing SUI. Usually, any injury or weakness to the pelvic floor muscles or the collagen(fascia) underlying the bladder and urethra.
Multiple pregnancies and childbirth. Especially, prolonged labours and large babies
- Aging and menopause due to loss of hormonal support
- Previous pelvic surgeries like hysterectomy, vaginal surgery etc
- Obesity
- Smoking
- Radiation treatment
- Persistent cough, chronic constipation can put strain on pelvic floor muscles
What are the details required?
- Thorough history is required regarding the normal voiding pattern and urinary leakage.
- Frequency of SUI in a day and the timing or activities it is associated with.
- The amount of urine that leaks per episode
- Whether needs to wear protective incontinent pads
- Quality of life
What are the Investigations?
- Examination
- Ultrasound scan
- Urine tests to rule out infection
- Urodynamics when required
Non-surgical treatment
Lifestyle changes
- Engage in regular exercise, which should include pelvic floor exercises.
- Steer clear of activities like high impact aerobics and jogging/running that put more strain on your abdomen.
- Quit smoking, which can make bladder weakness worse by making you cough. Avoid gaining excess weight. If overweight, a weight loss diet can help incontinence.
- Eat a balanced diet and drink enough water to keep bowels regular
- Limit the amount of caffeine to prevent bladder irritation and avoid increased urine production.
Weight loss
May reduce the incontinence to manageable levels without any further treatment
Physiotherapy
Both lifestyle modification combined with pelvic floor exercise gives 50 to 70 percent success rate when done under supervision of physiotherapist.
Needs commitment from the patient to do it regularly to see the benefit of it.
Atleast 8 contractions performed 3 times a day.
Need to try minimum for 3 months as a first line treatment.
This is a risk free management.
In approximately 1 in every 3 women these non-operative treatments are sufficient to cure or make your symptoms very much better.
Biofeedback
Artificial stimulation of the pelvic floor muscles helps to familiarise patients with pelvic floor contractions. A training method called biofeedback might enable you to identify the right muscles. In one type of biofeedback, sensors that detect the force of pelvic muscle contraction are inserted inside or outside the vagina. The measurement will be displayed on a monitor when the appropriate muscles are contracted.
What are pelvic floor muscles?
From the pubic bone in the front of the pelvis to the coccyx and sacrum in the back, the layers of muscles extend outward like a hammock. They close the bladder and bowel outlets and support the bowel, bladder, and uterus by being hard and supportive. The muscles in your pelvic floor relax when you urinate or bowel movement. They tighten again to regain control after emptying.
Eat a balanced diet that includes fruit and vegetables to avoid straining your pelvic floor muscles from constipation or being overweight.
Adequate fluid intake - If you have urgency or frequency, stay away from tea, coffee, and carbonated beverages.
Your control will improve if you contract your pelvic floor muscles before lifting heavy objects or before you cough or sneeze.
If your issue is urgency, contract your pelvic floor whenever you feel the urge to urinate and wait until the urge has passed before moving.
Oestrogen supplements
May help women with incontinence due to post-menopausal tissue atrophy
Drugs - there are now some drugs available which can temporarily improve incontinence, although they may not actually cure it. Success rate is 50% but side effects can be troublesome.
Laser therapy
Laser therapy is a new method of treating SUI. This is for SUI that is mild to moderate.
Disorders impacted by collagen damage have been successfully treated using laser therapy.
collagen production is encouraged by non-ablative laser therapy in the tissues near the bladder outflow.
These have already shown outstanding safety records, as well as improvements in the endopelvic fascia's connective tissue and SUI symptoms in SUI-affected women.
Surgical treatment
The main types of surgery include the following.
- Tape procedures. In this procedure a piece of mesh tape is placed under your urethra to support it, and the ends pulled through two small cuts either in your lower abdomen (tummy) or groin.
- Colposuspension. In this procedure your surgeon will lift the neck of your bladder by stitching the top of your vagina to the back of your pubic bone.
- Sling procedure. This procedure is similar to the tape procedure. But rather than using an artificial mesh, your surgeon will use a piece of your own tissue as the sling to support your urethra.
- Injections of bulking agents into the wall of the urethra. This narrows your urethra, helping you to hold urine in your bladder. The effects of this procedure may wear off over time and you may need to have further injections.
- Having an artificial urinary sphincter inserted.
Each procedure comes with its own risks and benefits. It’s important to discuss these and any complications you might experience with your doctor before you agree to go ahead with the procedure.